Growth into new markets and service lines is a cornerstone of strategic planning for health systems. Over the past several years, we’ve seen major systems make big bets on pediatric care as a promising avenue for growth, including:
A collaboration between Duke Health and UNC Health to build the first standalone children’s hospital in the North Carolina research triangle region.
The formation of a JV between CoxHealth and St. Louis Children’s Hospital to expand pediatric care in southwest Missouri, including a new pediatric outpatient center and enhanced NICU.
Major investments in new facilities by dedicated pediatric systems, such as Arkansas Children’s $371M rural expansion plan and Shriner Children’s new $153M pediatric research facility in Atlanta.
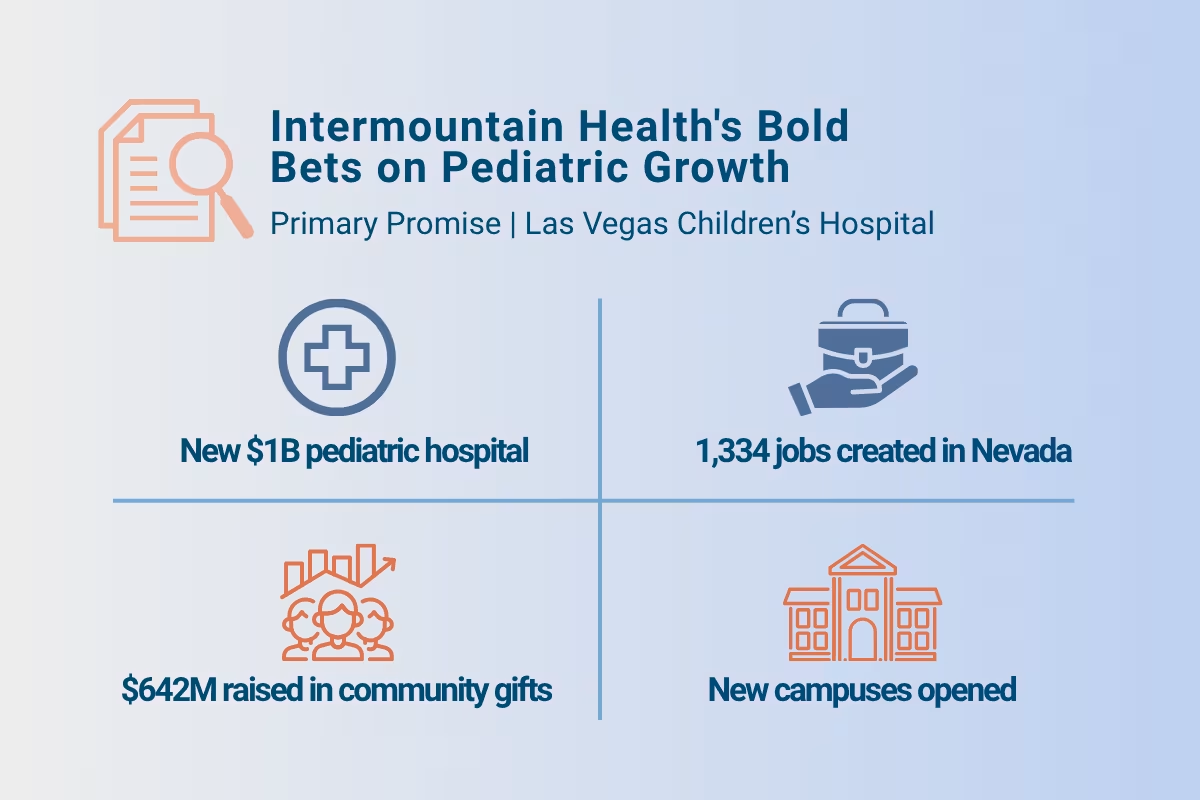
For this week’s Key Market Dive, we spoke with Intermountain Children’s Health AVP of Strategy and Business Development Mike Wecker to learn more about two of their recent efforts in the pediatric space: the construction of a new $1B pediatric hospital in Las Vegas and a $600M+ philanthropic fundraising campaign.
Why target pediatric growth?
Before we get into the case studies, it’s worth thinking about why so many systems see pediatrics as a worthwhile area for investment and expansion:
Community service: First and foremost, many health systems see pediatrics as a central part of their mission to serve the health and well-being of their communities.
Pediatric investment can also bolster brand visibility and foster goodwill that translates to philanthropic support (as we’ll see with our second case study).
Growing demand: In some parts of the southern U.S. “Sun Belt,” pediatric populations are seeing strong growth, driven by high birth rates and in-migration of young families. In other markets where pediatric populations are flat or declining, closures of smaller pediatric programs create opportunities for larger systems to capture and consolidate market share.
Medical advances are allowing children with chronic and complex conditions to live longer, creating sustained demand for adjacent specialty service lines like oncology.
Academic synergies: Children’s hospitals often serve as training hubs for residents and fellows, and pediatric specialties attract significant NIH and foundation research funding. Expanding pediatrics can deepen academic partnerships, enhance recruitment pipelines, and strengthen a health system’s position as a leader in innovation.
Competitive gaps: In many regions, there is no freestanding children’s hospital and only limited pediatric specialty capacity within community hospitals. Health systems that step into this gap can establish themselves as the default referral destination for complex pediatric cases, expand their catchment area, and create durable differentiation from local competitors.
On the other hand, multiple barriers discourage pediatric investment, including reimbursement challenges (especially with Medicaid) and staffing shortages. In the case studies below, we’ll discuss how Intermountain is leaning into growth opportunities while also finding creative ways to address these challenges.
Case Study #1: Intermountain’s new Nevada Children’s Hospital
In October 2024, Intermountain Health formally announced plans to build the first standalone children’s hospital in Las Vegas, projected to open by 2030.
The Intermountain Nevada children’s hospital builds on Intermountain’s growing presence in the region, which was jumpstarted in 2019 with the acquisition of HealthCare Partners Nevada. At the time, the physician group employed roughly 340 physicians and APPs at 55 clinics across southern Nevada, with a focus on Medicare Advantage patients.
The new Las Vegas children’s hospital represents both a response to community need and a strategic extension of Intermountain’s pediatric footprint. Las Vegas is the largest metropolitan area in the United States without a freestanding children’s hospital, forcing thousands of Nevada families each year to travel to Utah, California, or Arizona for specialized care.

A report by the consulting firm Tripp Umbach estimated that standing up the new campus would cost roughly $1B. An economic impact analysis by Intermountain projects that the hospital will create 1,334 jobs and generate $841M in annual economic output after the project is completed.
Here are the top takeaways from our interview with Intermountain leaders:
1. Favorable state policy changes helped make Medicaid reimbursement more sustainable.
For years, one of the biggest barriers to building a freestanding children’s hospital in Las Vegas was Nevada’s historically low Medicaid reimbursement rates. A disproportionately high share of the state’s pediatric population is covered by Medicaid, which meant that reimbursement levels would not come close to covering the cost of care delivery.
That dynamic shifted in 2023 when the state legislature, working with the Nevada Hospital Association, enacted a hospital provider assessment program. Under this arrangement, hospitals agreed to pay a fee on inpatient and outpatient revenues, which the state then used to draw down additional federal Medicaid matching funds. Intermountain leaders say this shift would dramatically improve the expected pediatric inpatient reimbursement.
2. The new hospital facilitates better care coordination for children.
By keeping care all within the same health system, care coordination occurs more seamlessly. It also enables families to return to Nevada more quickly when patients need to travel for care.
“Our goal is to keep as much care in Nevada as possible. We anticipate the number of patients that need to leave the state for care will continuously decrease as the hospital matures.” – Mike Wecker, Intermountain Children’s Health AVP of Strategy and Business Development
This approach benefits both ends of the system: Nevada families receive most of their care closer to home, while Intermountain’s Utah facilities can accept additional high-acuity cases that help sustain specialized programs to benefit patients with acute, complex needs.
3. Intermountain is taking an “all-of-the-above” approach to workforce development, with an emphasis on academic partnership.
Like many specialties, pediatric providers are in short supply, adding to the challenge of standing up a new children’s hospital. Intermountain told us they’re pulling every available lever to address the workforce issue: first by working with local physicians, supporting more local training, and recruiting physicians from out-of-state when needed.
In the long term, the system aims to support academic medicine broadly in Las Vegas and throughout Nevada to bolster their talent pipeline. Most of the physicians at Intermountain’s Primary Children’s Hospital in Salt Lake City trained at the hospital in partnership with the University of Utah.
“We are working with local academic partners to support the ongoing education and training of future physicians and caregivers. We see this as an important tool to increase the number of physicians in Nevada.” – Mike Wecker, Intermountain Children’s Health AVP of Strategy and Business Development
4. Nevada’s diverse population will help boost pediatric research.
Compared to Utah, Nevada is more racially, ethnically, and socioeconomically diverse. This diversity provides an invaluable opportunity to conduct pediatric research that better reflects the broader U.S. population, strengthening both clinical practice and academic credibility.
Case study #2: Intermountain’s “Primary Promise” philanthropy campaign
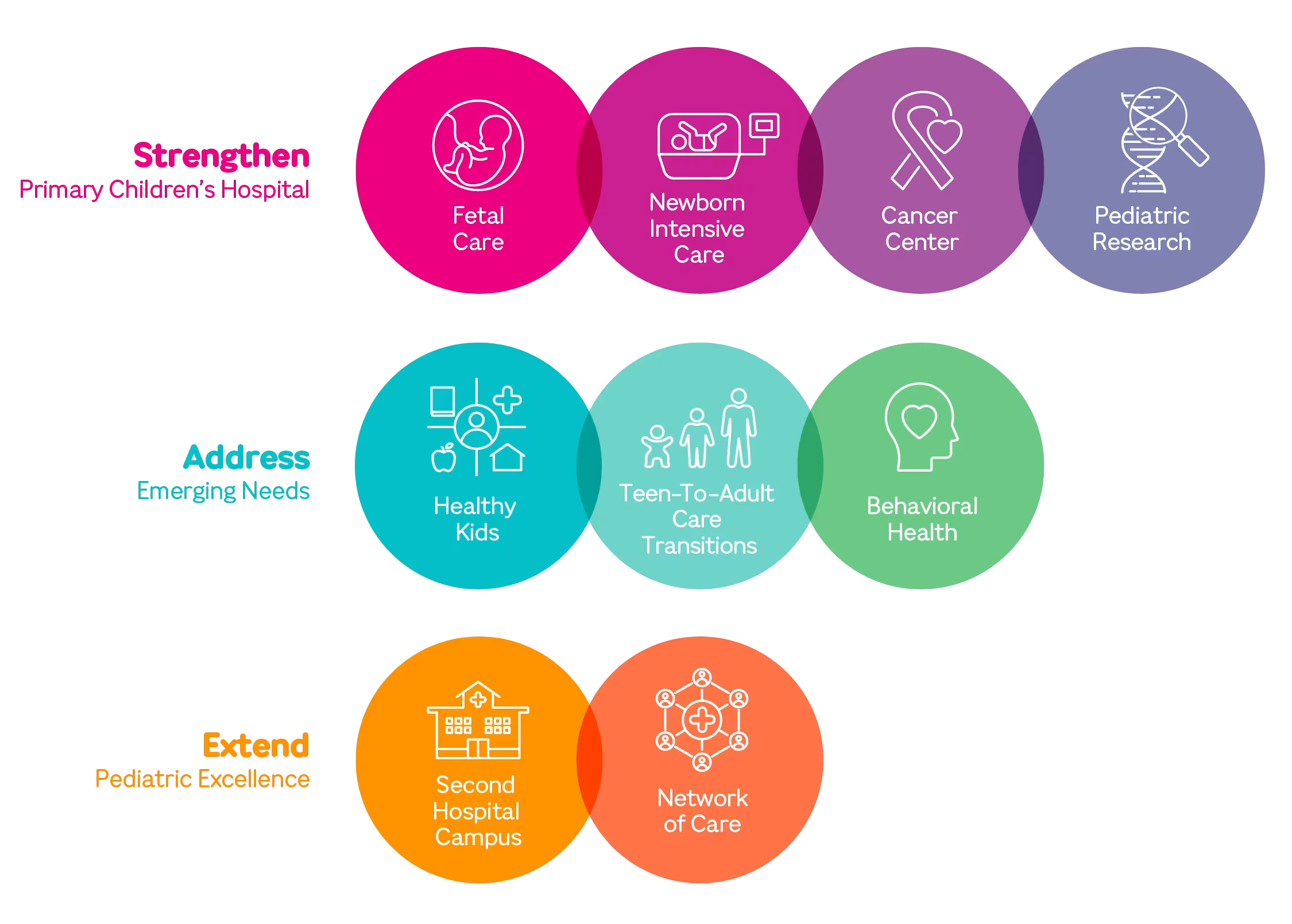
After years of discussion and planning, Intermountain publicly launched its Primary Promise philanthropic campaign to “build the nation’s model health system for children” in the Intermountain West in November 2022. Led by Intermountain Foundation, the campaign had an early goal of $500 million to bring its vision to life through a partnership between Intermountain Health and philanthropic members of the community. The financial target grew to at least $600M in response to community calls for more behavioral health services. In October 2025, Intermountain announced more than $642M in community gifts to the campaign.
To date, the funds have been used to strengthen the system’s flagship Primary Children’s Hospital with a renovated NICU, expand fetal care services, and upgrade a cancer treatment facility. The funds have also helped Intermountain extend their reach with a new pediatric campus in Lehi, Utah (opened in 2024), a new behavioral health campus in Taylorsville, Utah (opened in 2025), and expanded capabilities for telehealth and specialty care outreach. The campaign has also funded numerous other initiatives including a program to transition adolescent patients with chronic conditions into adult care.
In an interview, Intermountain identified several factors that have helped drive the campaign’s success. Here are our top takeaways:
1. Consolidating fundraising under a single foundation helped focus philanthropic efforts.
When the campaign was conceived, Intermountain’s philanthropic efforts were split across multiple hospital-based initiatives with a variety of fundraising goals. By consolidating these efforts into a single campaign, the system simultaneously scaled up its efforts and gave them a shared focus, enabling more transformative investments that serve an enterprise-wide vision.
2. Existing donor relationships helped build new connections with first-time donors.
In recent years, Utah has enjoyed a burst of technology-sector investment in the Salt Lake City and Provo areas, which have been colloquially referred to as the “Silicon Slopes” (a twist on “Silicon Valley” in California). This economic boom minted a new class of leaders, families and potential philanthropists. The Primary Promise campaign was led by four Utah civic and community business leaders — Gail Miller, founder, owner, and past chair of Larry H. Miller Company, and chair emeritus of the Intermountain Health Board of Trustees; Crystal Maggelet, chair and CEO of FJ Management Inc. and Intermountain Health trustee emeritus; Steve Lund, co-founder and executive board chair of Nu Skin Enterprises; and Spencer Zwick, co-founder & managing partner of Solamere Capital. Their leadership helped inspire a new generation of philanthropy to Primary Promise.
3. Priorities are mostly set by the system and the communities served, rather than donors.
Intermountain leaders emphasized that system and community needs define the agenda. Donor passions are welcomed, but philanthropic funds are steered toward strategically aligned priorities rather than one-off projects. By adopting a coordinated and systemic approach, the system ensures that philanthropic dollars have the maximum possible impact.
4. Philanthropic funds are used to catalyze new programs, not sustain them.
Intermountain leaders emphasized that Primary Promise dollars are spent on one-time capital investments and program startup costs, not permanent subsidies. New facilities and programs are expected to establish their own sustainable revenue streams and transition onto Intermountain’ standard operating budget. Ultimately, this keeps the system disciplined about long-term financial sustainability while ensuring that these investments are going towards transformative activities.
5. Value-based savings are limited for the pediatric population, but philanthropic dollars can still enable longer-term investments in health.
Unlike adult populations where investing in early or preventive interventions can reduce the likelihood of future high-cost procedures, pediatric populations offer fewer near-term cost-saving opportunities. Most children are healthy, while those with costly conditions are often born with them.
“You can keep kids with asthma out of the emergency room. That’s good for the child, and lowers the cost of care… but we’re talking about saving nickels where the adult system is talking about saving dollars. Our goal is to keep kids healthy, address underlying factors impacting health, and, when needed, provide the best acute care in the nation.” – Mike Wecker, Intermountain Children’s Health AVP of Strategy and Business Development
As a result, there are fewer opportunities for value-based contracting with payers for pediatric populations, adding to the challenge of financial sustainability. With that said, Primary Promise investments aim to address long-term drivers of health like immunization and nutrition to build healthier future adults, even if the financial return may not be realized for decades.
Our final thoughts
Pediatrics is an opportunity for strategic growth and furthering the mission that nonprofit health systems have to serve their communities. Intermountain’s experience shows that bold pediatric bets require more than good intentions—they demand policy conditions that make care sustainable, partnerships that build workforce pipelines, and philanthropy that sparks innovation without creating long-term dependency. While not every system is well-positioned to follow this exact playbook, their experience serves as a useful point of comparison for others looking to make moonshot bets in pediatrics or other service lines that can anchor facility expansion and strategic growth.