The biannual forums are a prime opportunity for strategy leaders to compare notes on the nitty-gritty details of their jobs. This year’s fall forum featured multiple presentations from CSOs diving deep into the specifics of their strategic planning cycles and how they’re responding to new financial and policy risks on the horizon.
Banner Health’s SVP of Finance Adrienne Moore (soon transitioning to a role as Banner’s strategy leader) led a session on aligning risk and strategy in the aftermath of the OBBBA legislation passed earlier this year. She was joined at the front of the room by 1m co-founder Chris Giuliano, who discussed how Banner Health is using his company’s risk management platform to quantify financial impacts from hundreds of potential policy shifts and market trends. In addition to federal policy headwinds, the framework also covers other risks like hurricanes and cyberattacks.
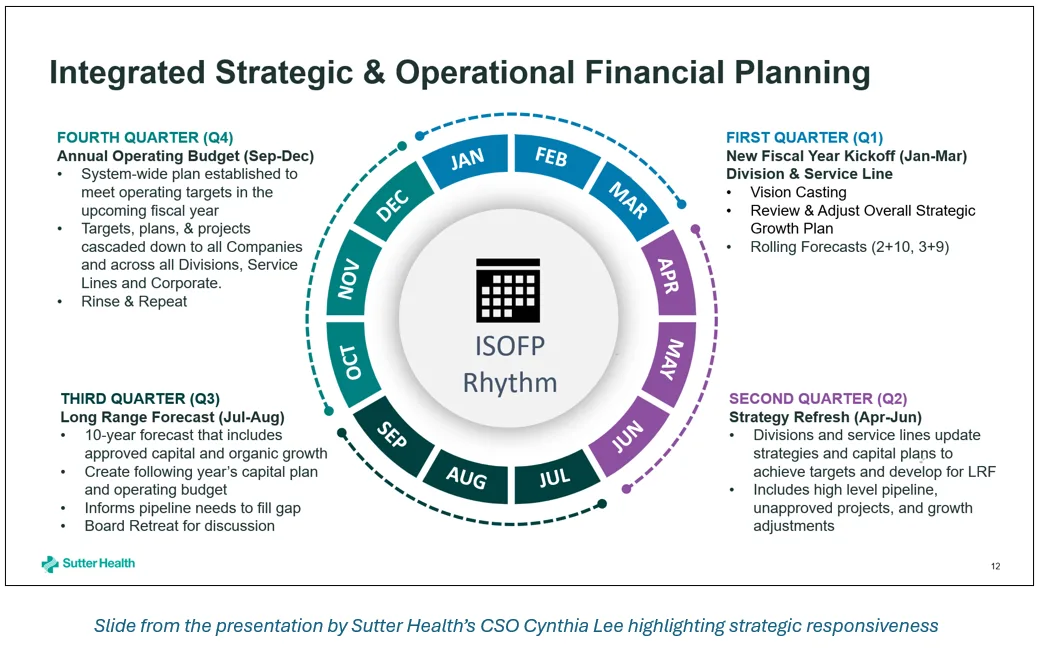
A second session on the shifting strategic landscape featured presentations by Mass General Brigham’s CSO Andy Shin, Sutter Health’s Chief Strategy and Growth Officer Cynthia Lee, and Sentara Health’s CSO Megan Perry. Among other topics, the three strategy leaders discussed optimizing service lines for long-term financial sustainability, strategic differentiation with a consumer-focused lens, and adjusting long-term strategic plans to account for near-term pressures and changes.
Key themes and insights
Across these two sessions, we heard a number of shared themes:
1. Quantifying risk can help make implicit assumptions more explicit.
Participants debated the value of detailed financial modeling for strategic planning. Many CSOs agreed that quantifying specific risks can help guide scenario planning and unlock new capabilities like sustainability testing and risk-based ROI frameworks. But participants also acknowledged that “every number is an assumption” and the risk of false precision.
CSOs also discussed how you model the strategic risk of sticking with the status quo. While the simplest approach is to create a baseline projection for the system’s financial trajectory, some participants worried that the interactions between different risks are too complex to model at this level of detail.
2. To keep fulfilling their missions, health systems need to plug a large financial gap.
The relationship between margin and mission is clear: if health systems can’t achieve financial sustainability, they won’t be able to continue caring for their communities. While many systems were already engaged in long-term efforts to optimize assets and cut costs, anticipated financial shortfalls driven by the One Big Beautiful Bill Act (also called HR1) have focused these efforts and created a more tangible and urgent timeline.
Health system strategic responses to shore up finances include outpatient growth, capacity/LOS optimization, provider-owned health plan integration, and AI deployment. To optimize service lines, Shin’s strategy team did a systematic analysis comparing MGB’s margins by service line to competing providers. Areas where other providers make margin but MGB doesn’t are potentially ripe for partnerships.
3. CSOs are trying to be more flexible and responsive with their planning.
Strategic plans that set goals for longer time horizons (5+ years) need to be frequently reassessed and adjusted in response to market and policy changes. Some systems are moving towards shorter and more flexible planning windows in response to volatile market conditions over the past several years (a trend we also noticed earlier this year in our Strategic Plan Compendium).
Moore also discussed using 1m’s platform to generate financial risk analysis on the fly when CEOs or board members email her about headlines in the news. Even if these estimates rely on numerous assumptions, having an initial number to work with gives health system leaders a more consistent framework for prioritizing risks.
4. Local factors can amplify shared challenges that all health systems face.
Health systems in different states face unique challenges—such as Massachusetts’s unique reliance on medical research funding, and California’s regulatory framework for earthquake mitigation. CSOs also discussed the varying degrees to which they depend on 340B: losing drug savings would be a tough (but survivable) blow at some health systems, but an existential threat at others.
While some systems are more vulnerable to certain threats than others, many headwinds affect the entire provider ecosystem (e.g., sharp increases in the uninsured rate or broad changes in population health). Every health system has its unique challenges, but there was also a sense of shared struggle at the forum.
5. Simplicity can be a strategic differentiator for internal and external stakeholders alike.
Lee discussed how Sutter Health consolidated 39 different physician incentive plans into a single plan that emphasizes growth. This new approach simplified the administrative burden across the system and created better alignment with the system’s strategic goals.
Likewise, Perry discussed how Sentara’s consumer-focused strategy leverages enterprise-wide care coordination and personalization to reduce frictions for patients. Emphasizing simplicity helps the system’s provider-led health plan differentiate itself from rival plans offered by national payers.
Our final thoughts
Taken together, the discussions underscored a shared determination among strategy leaders to confront mounting uncertainty with greater analytical rigor, operational agility, and a renewed commitment to sustaining their missions in a rapidly shifting landscape. Strategic planning pushes health systems to think about the medium and long term, but strategy leaders also need to continually refresh their thinking to stay tethered to reality.
