Introduction
In health system boardrooms, executives laud AI as a key enabler to addressing labor shortages and unsustainable nursing workload. But none of that transformation is possible without buy-in from frontline staff. Read on for the results of our 2024 survey of bedside RN sentiment on AI, safe staffing, and care model redesign—and the concrete opportunities for executives to better communicate AI's potential.
Key Takeaways
RNs aren't excited about AI solutions, but they are more ambivalent than actively opposed.
RNs’ primary concerns reflect a lack of confidence in AI’s ability to support safe care delivery, rather than a reluctance to change workflows.
RNs are far more receptive to solutions that automate administrative work like documentation and routine patient education—as opposed to those that would impact their clinical workflow or schedules.
Sharing key data about the nursing workforce and AI outcomes can substantially change staff readiness for AI.
Research Methodology
Overview of Nursing Catalyst 2024 RN Survey on Safe Staffing, Care Transformation Sentiment
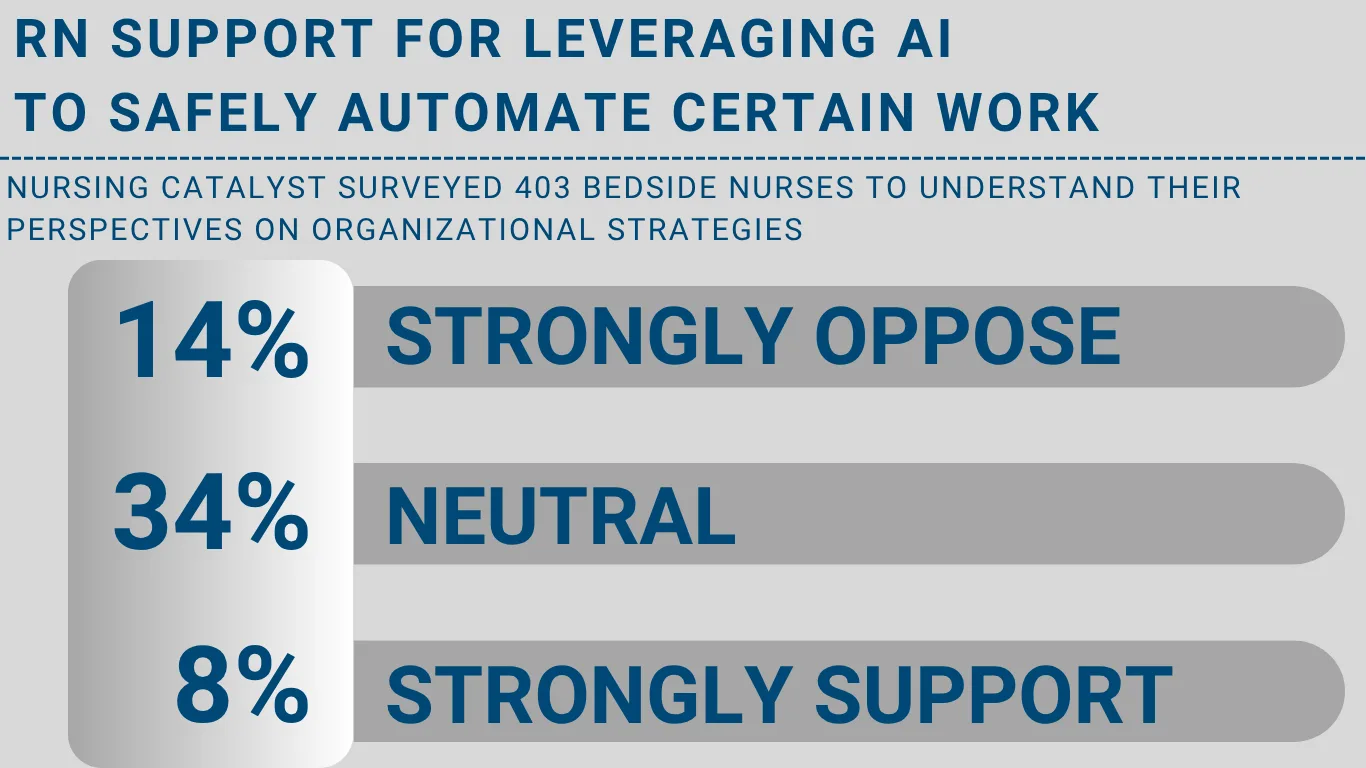
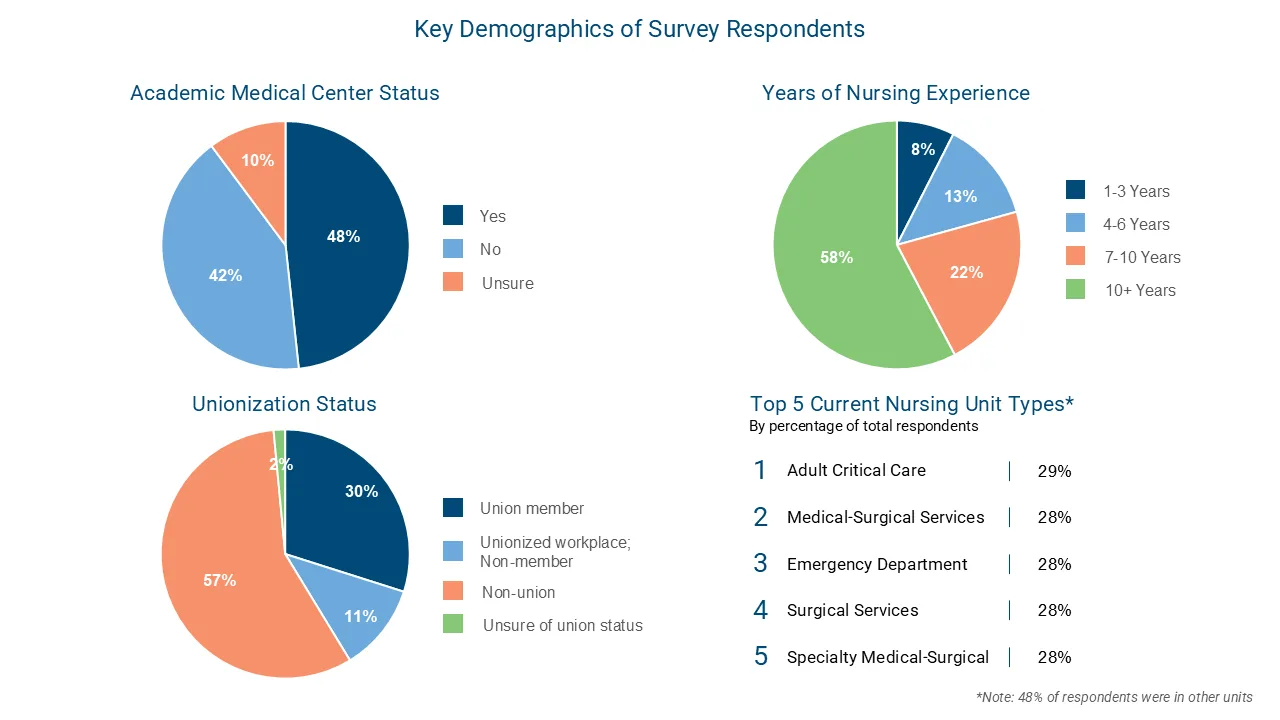
In Summer 2024, Nursing Catalyst surveyed 403 bedside nurses to understand their perspectives on organizational strategies to bolster safe staffing (including AI automation). Survey participants represented a range of ages, years of experience, clinical specialties, and AMC and union statuses.
Researchers supplemented the survey data by collecting further qualitative feedback during four focus groups with frontline nurses (n=41).
The goals of this research were:
to determine RN sentiment about current staffing levels and preferences among organizational strategies to maintain safe staffing
to gauge RN receptivity to and concerns about new models of clinical practice, including virtual nursing and AI-augmented tools
to understand what sources of information about nursing news and practice RNs trust, and
most importantly, to identify opportunities for nurse executives and other health system leaders to better communicate with their frontline.
This report is focused on a subsection of the findings related to frontline nurse sentiment towards AI, including receptivity to AI clinical solutions, concerns regarding AI use within bedside care, and preferences between different AI use cases.
What is Message Testing?
In addition to measuring baseline RN sentiment on AI and safe staffing, researchers also wanted to understand how changeable those perspectives are. To do so, they employed a market research technique called message testing. This method evaluates how specific communications impact an audience’s views, so leaders can evaluate the effectiveness of their communication strategy before they widely disseminate.
The message testing process consisted of three key stages:
Pre-Testing: Researchers surveyed participants to gauge their baseline support for various solutions, including mandated nurse-to-patient ratios, team-based care, virtual nursing, and artificial intelligence.
Exposure to Messaging: Respondents reviewed fact sets with information on sample outcomes, nursing supply and shortages, nursing workload, the impact of nursing supply on patient care quality and access, and the effect on health system financial sustainability.
Post-Testing: After exposure to these fact sets, researchers measured participants' support for the same solutions to identify any shifts in perception.
What Do RNs Think about AI in Clinical Practice?
RNs aren't excited about AI solutions, but they are more ambivalent than actively opposed.

Current media narratives suggest that bedside nurses are near-uniformly opposed to leveraging AI in clinical care—typically for fear of job loss or reduced agency in patient care decisions. These narratives are fueled by the high-profile Kaiser strike earlier this year where nurses held signs reading “Trust Nurses, Not AI” and criticized what they called “untested and unregulated” AI technologies.
However, the survey data indicate that RNs are more ambivalent than actively opposed to AI solutions. While they aren’t yet sold on AI’s ability to transform nursing practice—only 9% said they believed AI could help organizations maintain safe staffing levels—RN sentiment is largely neutral. The vast majority (78%) of survey respondents were either neutral to the idea of their organization implementing AI tools, or they only had slight positive or negative inclinations.
In other words, nurses' attitudes towards AI are not particularly polarized. Media or organizational narratives that depict nurses as AI detractors are at best inaccurate, and at worst a self-fulfilling prophecy in which the narrative itself suggests to nurses that AI technology is harmful.
Bottom line: We see a workforce that needs more information but is open to change.
Early-to mid-career nurses are the most receptive to AI.

When analyzing AI sentiment by nursing tenure, nurses with 4-6 years of experience show the highest level of support for AI implementation. 36% of this tenure group either somewhat (25%) or strongly (11%) support AI integration. Mid-career nurse openness to AI may stem from their balanced perspective: they have enough experience to feel confident in their clinical skills yet are still adaptable to workflow changes.
While both new graduate and experienced RNs reflect the ambivalence of the overall population, their sentiment also reflects the unique experiences of their tenure:
While a smaller percentage overall support AI (only 27%), new graduates have the highest level of strong support (13%) of all tenure groups. This dichotomy might reflect a mix of enthusiasm for technology-enabled innovation among tech-savvy recent graduates and the challenges of integrating new technologies while still mastering fundamental nursing skills.
Interestingly, the most tenured nurses (10+ years) demonstrate the highest level of ambivalence. 39% neither support nor oppose AI. This neutrality might indicate a "wait-and-see" approach, reflecting their extensive experience with labor-intensive technology adoptions (such as the EHR).
Union status does not impact AI support.

Despite the widely publicized nursing union strikes against AI integration, there is no difference in overall support between unionized (28%) and non-unionized nurses (28%).
RNs’ primary concerns reflect a lack of confidence in AI’s ability to support safe care delivery, rather than a reluctance to change workflows.
The survey results paint a clear picture: nurses' concerns about AI center on its impact to clinical care rather than its potential to change nursing workflow. Of the five major areas of concern identified, the top three focus on patient safety, care quality, and professional practice integrity. Notably, traditional change management concerns like workflow disruption and technology adoption ranked significantly lower. Below are nurses' key concerns, ranked by prevalence.

Patient Care Quality and Experience
An overwhelming 73% of respondents cited AI’s (potentially harmful) impact to patient care quality and experience as their top concern. RNs worry that AI lacks the human intuition and holistic perspective needed for safe patient care, expressing particular concern about AI's inability to recognize subtle clinical changes or have the "gut feeling" that can guide critical decisions in care. Another key concern is that automating tasks that have traditionally been done by bedside staff could erode the patient care experience. Here's what our respondents had to say about the impact of AI on patient care quality and experience:
“Concerns about the accuracy of AI generated content”
“Lack of AI to see full picture in patient care”
“Inability for technology to pick up on things that only humans have such as the 'gut feeling’"
“Concerns about patient perceived experience”
Trust and Reliability
59% of nurses report concern about AI accuracy and data integrity, with specific concerns about algorithmic bias, false alerts, and error rates. RNs fear both the direct harm that inaccuracies could have on patient care and the professional consequences that could result from harm—particularly the risk to their nursing license. These concerns are amplified by their experience with existing clinical alerts that generate false positives or are too frequent to allow for bedside intervention. Here's what our respondents had to say about the impact of AI on trust and reliability:
“AI is not infallible, and I'm concerned about who is to blame if it makes a mistake. (It's always the nurse's fault in the end.)”
“AI not reliable”
“We already have some *Alerts* from the computer and most people just ignore them because most of the time we already are aware or it is falsely flagging things.”
“Inaccuracy”
Erosion of Nursing Profession
Anxiety about AI’s impact on nursing jobs extends beyond weakened job security: 55% of RNs worry about losing the agency to make critical patient care decisions. These comments reflect a fear that AI could fundamentally alter nursing roles and work—or minimally erode the ability of nurses to see the whole patient and/or critically think. Here's what our respondents had to say about the impact of AI on the erosion of nursing profession:
“Losing personal care and relationships with patients”
“Losing hands on experience”
“Concerns that it will reduce the ability for nurses to critically think”
Job Security
The fear of job displacement is palpable, with 55% of RNs reported feeling concerned about AI replacing bedside clinicians. These workforce concerns reflect a broader pattern, as professionals across industries wrestle with AI's potential impact on their roles.
Workload
Despite workload being a leading cause of nurse turnover and a top concern for nursing leaders, respondents ranked it lower on the list of AI-specific concerns. For example, workload-related concerns “disruptions to existing workflows” (40%) and “the need to learn potentially short-lived AI technologies” (30%) fell well below their concerns about clinical quality and reliability. Though there was less worry overall about a potential increase in workload due to workflow changes, respondents still expressed repeated concerns that automation broadly would be used as a justification to increase patient assignments. Here's what our respondents had to say about the impact of AI on workload:
“Hospitals using AI as reason to increase patient ratios”
RNs are far more receptive to solutions that automate administrative work—as opposed to those that would impact their clinical workflow or schedules.

RNs are the most receptive to AI solutions that offload administrative burdens and/or help nurses deliver care more effectively or efficiently—as opposed to those that might alter their core workflows or decision-making processes.
For example, the top-ranked AI applications are documentation-focused: voice-to-text documentation tops the list of desired AI solutions, followed closely by AI-translated care plans to match patient reading level and preferred language. Nurses also show interest in solutions that help them respond more quickly to rapid changes in condition, such as AI-powered sepsis alerts (ranked third).
AI applications that recommend nursing workflows and decision-making processes rank lower—even if the decision is still ultimately left to the nurse. For example, AI solutions that recommend care tasks based on acuity (ranked fourth) or distribute care tasks among the bedside team (ranked fifth) rank lower in terms of preferences. This suggests that nurses are not enthusiastic about the idea of AI dictating their workflow, even if it supports top of license work or creates team efficiencies.
The least preferred application is AI-powered scheduling recommendations. This lower ranking likely reflects nurses' desire to maintain control over their work-life balance and skepticism about AI's ability to handle the complex personal and professional factors that go into scheduling.
Said differently, nurses are most open to AI automating tasks that are below the scope of their license or that they would otherwise like to offload (e.g., documentation). Organizations looking to build widespread frontline AI buy-in should start there before moving on to solutions likely to face resistance.
Can We Sway RNs’ Perception of AI?
Staff perceptions of AI are highly changeable.

Low nurse confidence in AI’s ability to positively impact patient care can lead to assumption that these beliefs are strongly held. But when presented with relevant facts and information, nurses' support of AI implementation increases over 20 points. Before seeing the fact set, only 28% of nurses expressed some level of support. After exposure to the information, this support jumped to 52% - an increase of 24 percentage points.
This ranking reveals a crucial insight: nurses' ambivalence towards AI is not due to negative experiences with the technology, but rather a lack of exposure to meaningful outcomes data. The strong preference for real-world evidence suggests that nurses are open to AI solutions, but they need to see tangible results that demonstrate AI's effectiveness and impact on care quality.
Sharing key data about the nursing workforce and AI outcomes can substantially change staff readiness for AI.

When presented with different types of information about healthcare transformation, nurses find certain messages more compelling. Data about nursing workload resonates most strongly (44%), followed by information about how nursing supply impacts patient quality and access (37%). This suggests nurses are most receptive to context that connects AI implementation to addressing their day-to-day challenges and improving patient care.

When specifically asked what information they want about AI initiatives, nurses prioritize concrete evidence of success. Two-thirds (66%) want to see outcomes data from pilot testing, while 63% want to understand how systems monitor these outcomes. Nurses also highly value peer experience—58% want to connect with colleagues who have used the technology. Hearing from colleagues who have successfully integrated AI into their workflows can provide valuable, practical insights and help alleviate concerns. This preference for empirical evidence and peer validation suggests that healthcare organizations can build AI support by leading with quality outcomes data and facilitating peer-to-peer learning.
Healthcare leaders must prioritize visibility and direct communication about AI initiatives—especially CNOs.

Healthcare organizations should focus their AI communication strategy on mobilizing both frontline managers and CNOs, while recognizing the unique role each leader can play.
Managers are well-positioned to drive change, ranking as the third most common primary source of nursing news (42%) after nursing associations (74%) and colleagues (59%). Despite CNOs' current ranking as a primary source for only 27% of frontline RNs, there's significant room for greater executive engagement—61% of nurses shared they want to receive important information directly from their CNO.
To maximize leadership's impact on AI adoption, organizations should pursue two parallel strategies. First, equip frontline managers with detailed implementation information for day-to-day guidance. Second, create direct communication channels between CNOs and staff for strategic messaging about AI initiatives. This combination of hands-on support and executive visibility will help build staff confidence in AI implementation.
Looking for more research on how AI will impact Nursing? Stay tuned for our upcoming research in early 2025 on:
How to engage different archetypes within frontline staff when rolling out new AI technologies
Where AI is driving patient outcomes and improving nursing workload