Improving access to care was the number one priority of CFOs for 2024, as well as a top priority for CSOs and strategy leaders. But benchmarking access remains a challenge. Specifically, a lack of hard data makes it difficult for executives to compare their system’s performance with their peers and competitors, especially across different markets and scheduling channels.
This is compounded by the fact that most access reports only test call center scheduling and leave out the digital experience. Even oft-cited statistics, like Merritt Hawkins’ survey that it takes 20.6 days to get primary care in urban markets, only look at call wait times and thus build an incomplete picture of the full patient experience.
Our Strategy Catalyst team has been hard at work to fill that gap. Building on our previous research, the Strategy Catalyst team spent the past several months conducting another round of “secret shopping” evaluations to test the availability of appointments at 52 health systems and four disruptor competitors (Walgreens, Carbon Health, One Medical, and Tia).
Last year, we tested the ability of consumers to secure a primary care appointment using digital self-scheduling capabilities. For this year’s evaluation, in addition to digital self-scheduling, we also tested the ability to schedule appointments over the phone via health system access centers.
Our key findings included:
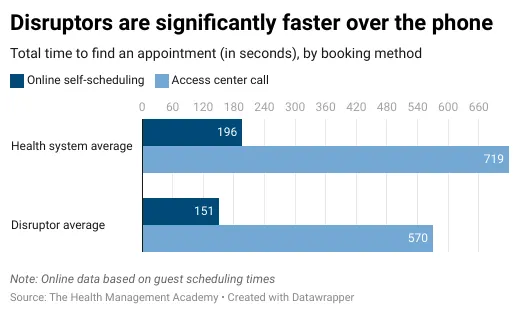
Online appointments offered care twice as fast: Across 52 health systems, our secret shoppers were able to get a primary care appointment within 7 days on average by using online self-scheduling, versus 16 days over the phone.
Disruptors still have a substantial edge with primary care access: All of the disruptors we tested offered next-day or same-day appointments online and over the phone. Overall access was 12x faster on average.
Disruptors had a more streamlined user experience: On average, our secret shoppers needed 32% longer to schedule an online appointment with health systems compared to disruptors (2:48 minutes vs. 2:07 minutes) and spent 60% more time on hold when seeking an appointment over the phone (3:11 minutes vs. 1:57 minutes).
In addition to primary care appointments, we also tested the availability of appointments for three specialties that drive significant downstream revenue: gastroenterology, imaging (mammography), and OBGYN. To bring you that data more fully, we’ll be focusing on primary care in this edition and will dive into the results with specialty access in our next issue.
This issue will first cover our methodology, then walk through our experience scheduling:
An appointment online with a guest account
An online appointment online with a logged-in account
An appointment over the phone
We’ll compare the experience between health systems and “disruptors,” call out several top performers across our members, and end with several strategic recommendations informed by the work.
Why phone calls are so important for access
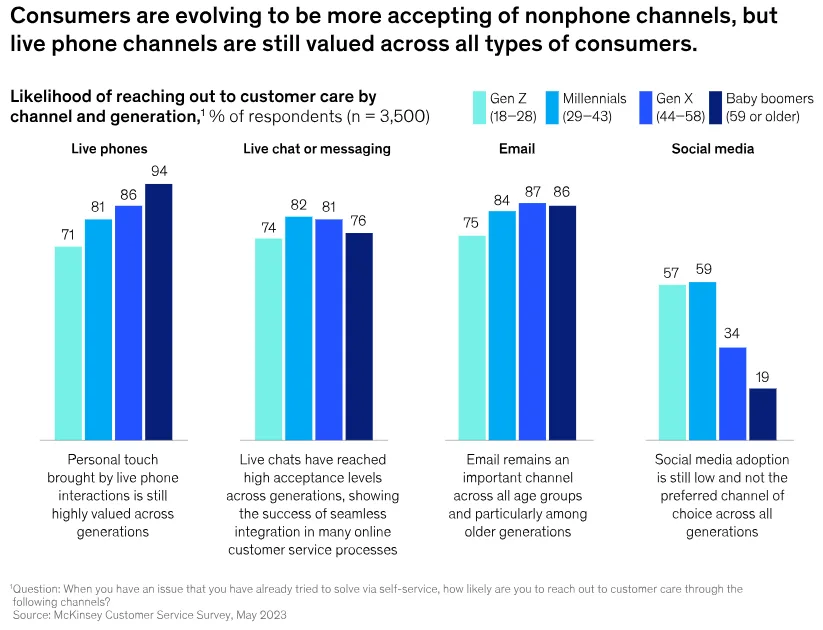
Given the health system focus over the past few years on digital self-scheduling, we initially chose to focus only on that channel last year. However, we heard clearly from members that phone channels were still vital as a marker for access. This is borne out by data. According to a survey by Kyruus Health, 41% of healthcare consumers still prefer to schedule new patient appointments over the phone, compared to 38% who prefer to schedule online.
Interestingly, this preference cuts across generations. Contrary to stereotypes about younger “digital native” consumers, a 2023 survey by McKinsey found that 71% of Gen Z consumers say they’re likely to reach out for customer service over the phone, making it nearly as popular as alternatives like live chats or email. McKinsey cites one financial-services company which reports Gen Z is 30-40% more likely to call than even millennials.
But the phone experience often isn’t meeting consumer needs. Many consumers report frustration when they try to book a healthcare appointment over the phone. In the same Kyruus survey mentioned above, 50% of consumers said they couldn’t book an appointment in a single call, 64% said they lacked confidence that their appointment was booked with an appropriate provider, and 22% reported long hold times.
We encountered many of these same difficulties. At the conclusion of this deep dive, we’ll share our recommendations for best practices to avoid these pain points.
How our “secret shop” process worked
To establish an industry baseline, we conducted our secret shopping evaluation for 52 health systems (all voluntary opt-ins) and four competing disruptors: Walgreens, Carbon Health, One Medical, and Tia. These four disruptors were selected because they have a national presence with primary care capabilities (last year’s evaluation included Walmart Health, which has since been shuttered). Walgreens’ website redirected us to VillageMD, so our evaluation reflects our experience seeking an appointment with them.
Our evaluation is a snapshot in time: we tested all health systems and disruptors over a six-week period in late April and May.
The health systems in our cohort had net patient revenue ranging from $500M to $20B annually; 16 of them were AMCs. Health systems in both rural and urban areas participated, and every region of the contiguous U.S. was represented.
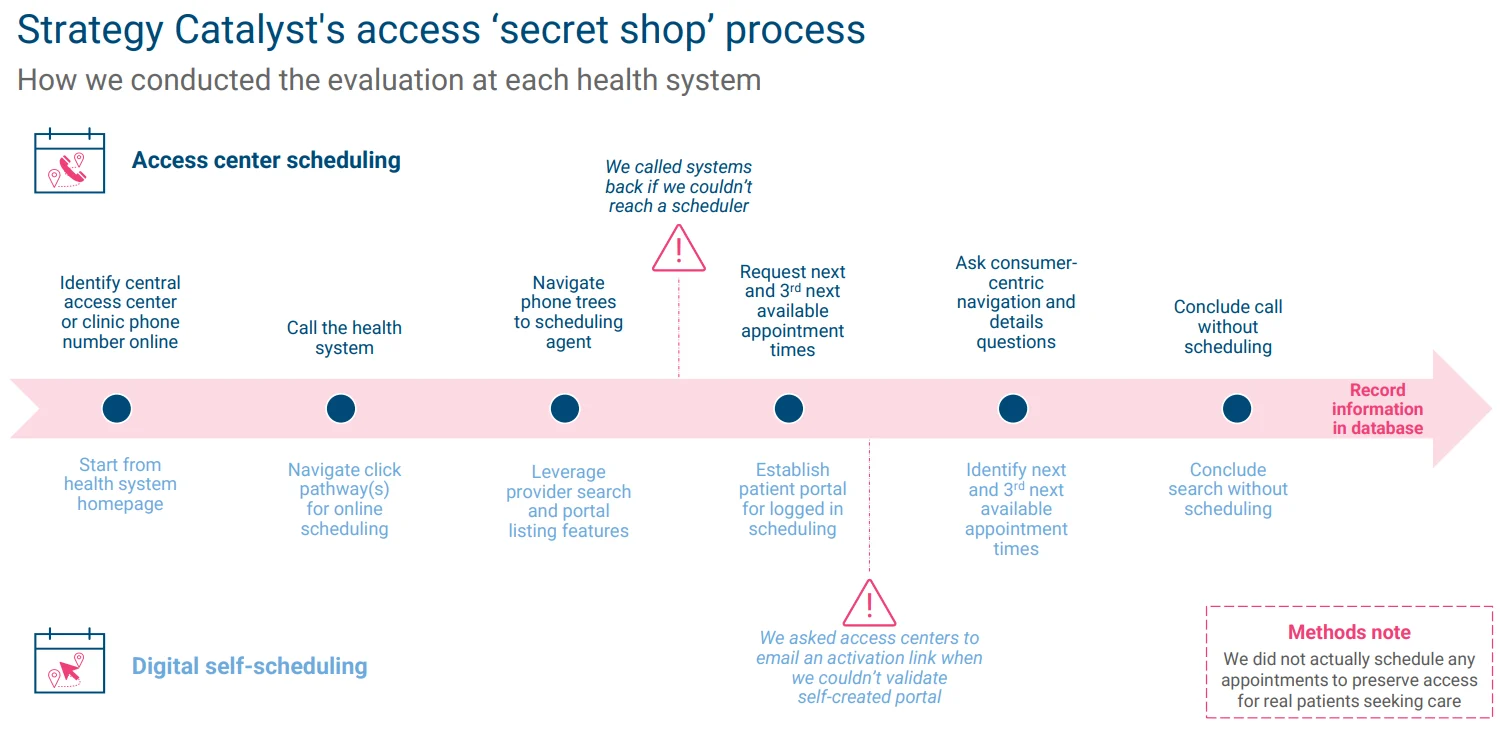
As shown in the diagram below, we established parallel processes for seeking in-person primary care appointments at each health system over the phone and online. We tracked the total amount of time it takes to obtain an appointment, noted the presence of any barriers (e.g., call transfers or “digital dead ends”), and measured access by determining how many business days our hypothetical patient would need to wait for the first- and third-next-available appointments.
The results: Most health systems are on par with disruptors when it comes to digital self-scheduling access
Our first evaluation tested the experience of a hypothetical consumer seeking a primary care appointment online with a “guest” account.
We were able to conduct this test for 41 of the health systems in our cohort and two of the four disruptors. One Medical, Tia, and 12 of the health systems we evaluated require users to log-in and were therefore left off these results.
Our results suggest that the median health system is roughly on par with Carbon and Walgreens in terms of days until an available appointment. However, a number of systems with long waits dragged up the health system average.
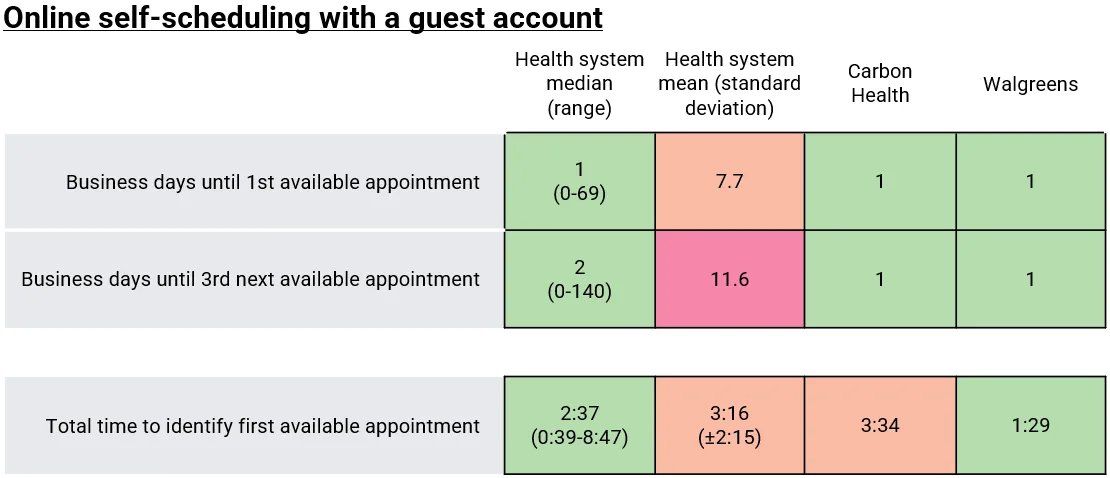
In total, four health systems—Advocate Health, Corewell, Ohio State University Medical Center, and Piedmont Healthcare—offered same-day appointments, while 22 systems offered next-day appointments. In contrast, at four of the systems we tested, the next available appointment was more than 40 business days (or 8 weeks) away.
Health systems were also competitive with the disruptors in terms of the total time needed to identify an appointment, a measure we use as a proxy for ease-of-access. We were particularly impressed with Advocate Health: we were able to find an appointment within 39 seconds of opening their website with the aid of an easy filtering interface and a calendar view of the soonest available appointments.
We were also impressed that 90% of the health systems we tested offered appointments on weekdays outside normal business hours. In our view, this is a key convenience for many consumers who don’t have the means to take time off work to see a provider. Walgreens/VillageMD also offered such appointments to guests, while Carbon Health did not.
As we conducted our evaluations, we also assigned each health system a net promoter score reflecting our impression of the user experience. Overall, 13 health systems and Walgreens scored a 9 or 10 (putting us in the “promoter” category), while 17 health systems scored a 6 or below (putting us in the “detractor” group). The mean NPS across all health systems we tested was 7.2. VillageMD (through Walgreens) achieved a 9 out of 10 on our NPS measure because their platform was easy to use, highly responsive, and offered lots of near-term availability with appointments outside normal business hours. Carbon Health received an NPS of 8.
Our second evaluation tested the same metrics with our secret shopper logged into an existing account in the digital self-scheduling interface.
We were able to conduct this test for 22 health systems and three of the disruptors. The remaining 30 health systems and Walgreens were not tested because we could not activate a patient portal (e.g., MyChart) or because the new patient portal did not provide direct access to scheduling.
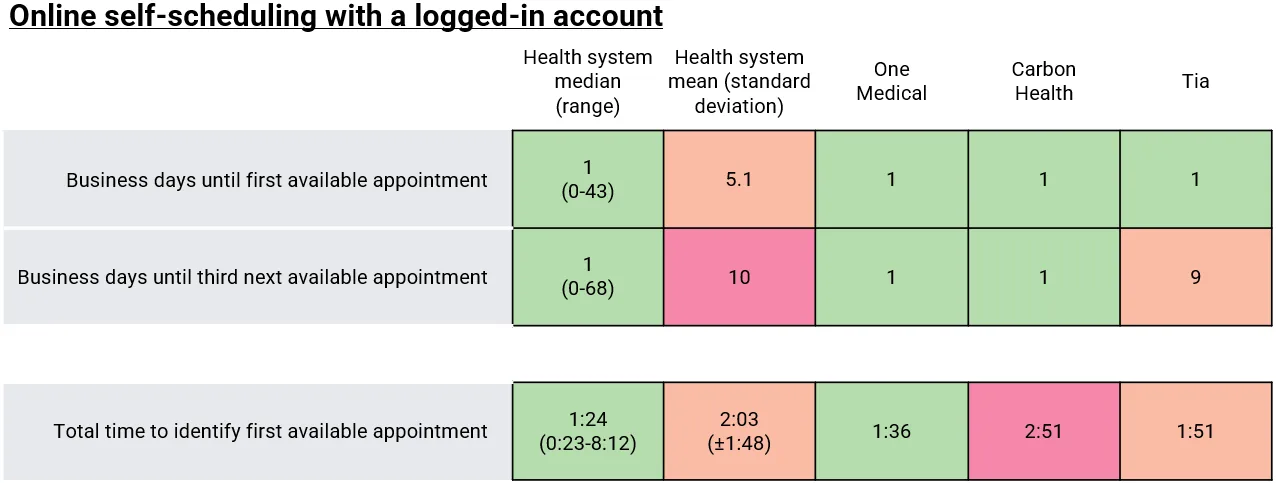
Our results were broadly similar to the first guest log-in evaluation in terms of time until the first- and third-next-available appointments, although it was notable that Tia’s third-next-available appointment was more than a week away.
The biggest difference was the amount of time it took to navigate the website. On average, our secret shoppers spent 37% less time seeking an appointment when logged into a health system website compared to the guest experience. Our fastest experience (23 seconds) was with Cox Health, which offered many more potential appointments to our logged-in shopper that were not visible to the guest account.
The disruptors were a mixed bag on this measure. Carbon Health was particularly slow because our secret shopper was forced to click into multiple locations to look for the soonest available appointment, with no easy way to compare across locations. In contrast, One Medical’s interface listed all available appointments across multiple providers in one view.
Access center results: Disruptors offer a superior experience over the phone
Our third evaluation tested the ability to secure an appointment by calling into an access center and asking an agent to find options.
We were able to conduct this test for 47 health systems in our cohort and three of the four disruptors (Tia did not offer the ability to seek an appointment over the phone). For the remaining five health systems, we were unable to complete our evaluation due to telephonic dead ends or because they were not accepting new patients.
We started this evaluation by using Google to locate a phone number for each health system’s access center. This was not always easy: in some cases, we were forced to call a hospital’s main listed number and request a transfer to the appropriate department. The best performing systems clearly advertised a single phone number for their access center with posted hours of operation.
Overall, the access centers managed by the three disruptors outperformed the health systems’ by most measures.
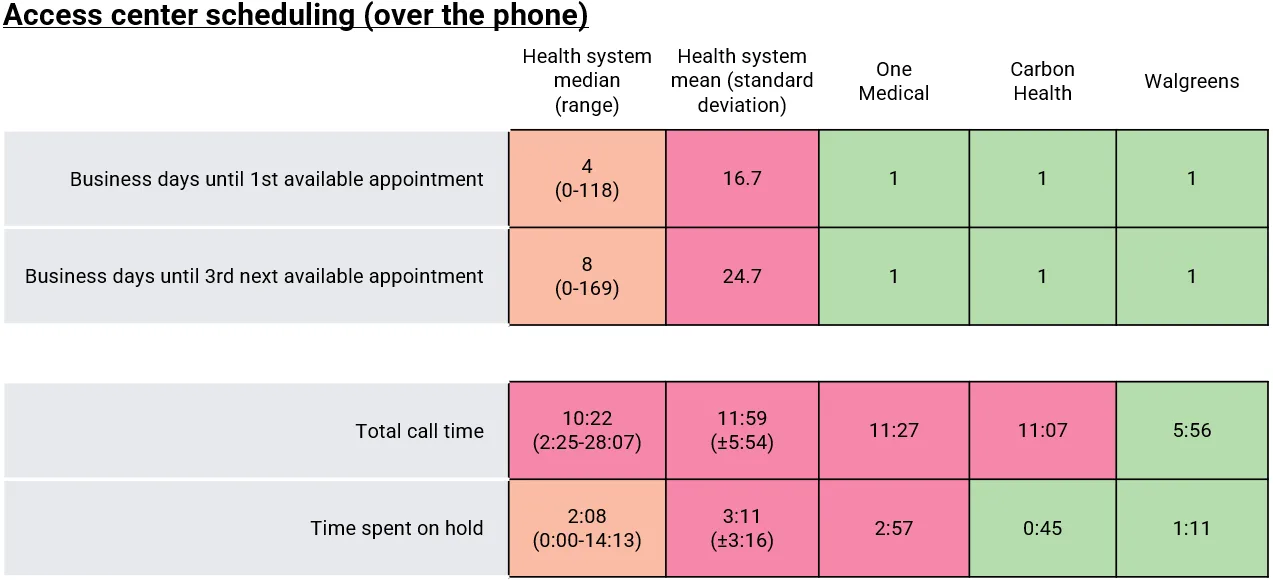
All three disruptors were able to offer next-day appointments over the phone, whereas agents at most health system access centers were only able to find appointments several days out. This gap was even wider for the third-next-available appointment.
There was wide variation in total call and wait times. Walgreens offered the fastest call experience because their agent was willing to share possible appointment times without asking our shopper to share detailed patient demographics. In contrast, Carbon and One Medical (and most of the health systems we called) required our secret shopper to give information like address, phone numbers, and even social security numbers before offering appointment times.
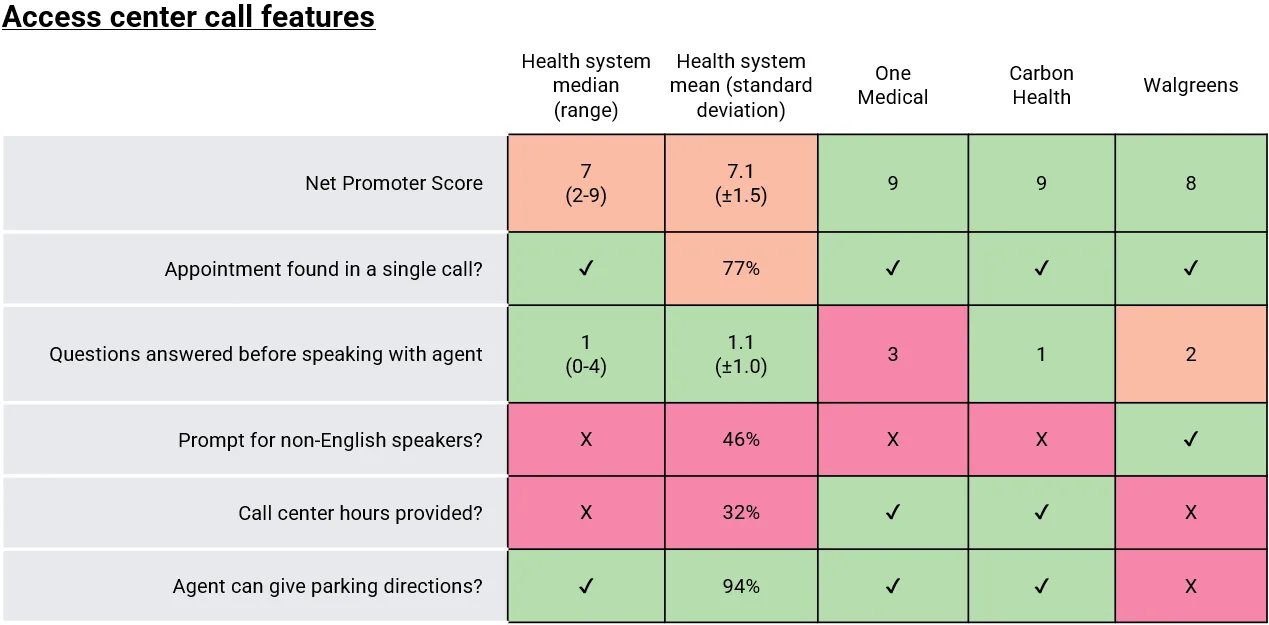
One of the biggest differentiators between high-performing and low-performing health systems was the ability to find an appointment in a single call. We found the experience extremely frustrating when we were forced to make several calls and repeat information to multiple agents, resulting in lower NPS scores for certain health systems.
In some cases, our call was transferred three or four times before we were connected with an agent capable of finding bookings. This greatly lengthened the overall amount of time we spent on the call (in the worst cases, it took us more than 20 minutes to find an appointment over the phone). These low performers in terms of total wait time brought up the mean substantially from the median.
More than half of the health systems we tested (and two of the three disruptors) failed to provide a prompt for non-English speakers. We think this is a key accessibility feature, although we also understand that language needs vary by region.
Overall, we gave the three disruptors higher NPS scores than most of the health systems we tested. Two disruptors (One Medical and Carbon) and eight health systems received a score of 9. We were particularly impressed with how helpful and knowledgeable Inova’s access center agent was, and we were also impressed by the extended hours (7am-8pm on weekdays, 9am-5pm on weekends) offered by Lehigh Valley Health Network’s access center.
So What?
1. The delta between online and calling access shows a need to improve access center scheduling capabilities.
In most cases, the online self-scheduling interface offered significantly sooner appointments than the access center we called at the same health system.

We know that this is intentional at certain systems to encourage patients to use digital capabilities (e.g., schedulers “save” slots for digital access). But we don’t think that these slots would explain the whole difference—especially across 50+ systems. In our view, this suggests that access center agents often do not have full access to a “birds-eye view” of all available appointments. For instance, they may have to toggle in between different sites or clinics which can limit their overall view of availability. Better integration of scheduling tools for call center agents seems like an important priority (even if it’s not necessarily a light lift).
In terms of governance, we speculate that this gap exists in part because online self-scheduling capabilities are often managed by a dedicated team that has been prioritized as part of a broader digital transformation, whereas access centers and phone lines are built on legacy systems that haven’t had the benefit that a digital transformation usually provides. This is especially apparent at systems that do not clearly advertise a single access center phone number. We were surprised how often this single line was not clear.
Our recommendation is that systems should take a holistic, multi-channel approach to appointment access so that consumers have a consistent experience regardless of their preferred means of contact.
2. Adding other “quality of life” features to access centers is low-hanging fruit.
More broadly, many health system access centers would benefit from adopting the best practices we saw adopted by some peers and disruptors.
First and foremost, as just mentioned, health systems need to have a single consolidated phone number for their access center that is easily identifiable on the health system website and on Google Maps. Some of our most time intensive experiences were with systems that forced us to call around multiple facilities before finally directing us to an agent who could actually help.
Many systems would also benefit from a callback feature for customers that don’t want to sit around on hold for extended periods. In some cases, we were even promised a callback that never occurred, forcing us to eventually call back ourselves. While we recognize that not all health systems have the staffing resources to avoid wait times altogether (especially during peak calling hours), this is a way to improve the user experience.
We also found a high degree of variability in agent responsiveness. Some call center agents more helpful than others, especially when we had questions about costs and visit logistics. In our experience, this is partly because some agents were better prepared with relevant information. But there’s also a culture component: some agents expressed a friendly and helpful attitude that stood out to our evaluators. Maintaining this culture is challenging—especially given that THMA surveys of CHROs have found turnover rates of 39% on average across health systems for call center staff and that 96% of call center staff report feeling acute stress on a weekly basis.
However, as many strategy leaders have to make hard decisions about outsourcing or offshoring call center staff, as well as make more exiting decisions about how intelligent automation can augment call center performance, we think it’s important to keep this data on patient experience top-of-mind. (For more information on how evaluators graded your particular system, please reach out to strategycatalyst@hmacademy.com for your custom report).
Ultimately, we think it’s critically important to ensure that consumers can make an appointment with a single phone call. Most health systems (and all disruptors) met this standard, but poor organization and training is still holding some back. Given that we know that 27% of all patients who face a dropped call will go elsewhere, a reliable patient experience can help prevent revenue leakage.
3. Disruptors are still setting consumer expectations, but health systems are catching up.
In last year’s evaluation, we were able to book appointments with One Medical, Walgreens, and Walmart significantly faster than the average health system. In this year’s test, the results were much closer. While we don’t have exact time differences due to methodology changes, this is good news for health systems.
The bad news is that there was still a delta. This year’s evaluation suggests that disruptors also have a substantial edge over the phone.
As we wrote above, many consumers prefer call centers over other forms of customer service. By offering a more convenient and responsive experience over the phone, these disruptors are potentially winning over new patients and setting consumer expectations.
The important point to note is that disruptors can rewrite these consumer expectations, even if their business models aren’t working overall. According to a leaked document, Amazon is expecting to lose $506M with One Medical in 2024. Its market cap is almost $2 trillion so it could lose 10x that every year—an amount that would sink all health systems. But millennials and Gen Z’s experience with care can still be shaped by their experience with One Medical. Similarly, as our experience with virtual care with now-shuttered Walmart shows where we were offered a prescription within 30 seconds of the phone call, even failed businesses can rewrite patients’ expectations.
We think this is essential for health systems to understand, even if not actively working on a strategy to “compete” with disruptors.
What’s next?
In this year’s secret shopping evaluation, we also tested the availability of specialist appointments online and over the phone for gastroenterology, imaging (mammography), and OBGYN care. Stay tuned next edition for another deep dive into our findings and more callouts for which systems did best with these scheduling pathways.
