Across Spring 2024, The Health Management Academy convened 30 Forums and Collaboratives for health system and industry executives from around the country to discuss their most pressing challenges, successes, and lessons learned.
In past issues of Academy360, we’ve outlined themes of some of these executive touchpoints—offering an overview of the role-specific conversations. However, we’ve rarely provided a summary across executives. Therefore, for this issue, we looked across audiences to give you an overview of what’s top-of-mind across the C-suite.
Here is a recap of the most recurring themes and topics discussed:
1. With financial longevity becoming a moving goalpost, almost every C-suite leader is focused on efficiency and standardization.
Increased pressure to improve operating margins and finance growth strategies have senior leaders doubling down on scaling operational efficiencies—often with the goal of greater standardization.
COOs unanimously agreed that their operations are not yet fully optimized, with M&A of the past few years often contributing to lingering integration challenges. Many are trying to intentionally align each internal effort and KPI back to the core system strategy.
CFOs are trying to drive more standardization and centralization by moving more services to shared services models. However, in tandem, legal and cybersecurity risk has limited some recent offshoring or outsourcing efforts.
CPEs are working towards clinical standardization by centralizing operating structures under the mandate that quality must be a system-wide priority. At one system, they clearly defined the role each clinical leader plays in quality improvement. At another, they trained medical directors and chairs on how to best work with nurse counterparts to uphold quality standards.
Senior leaders are also becoming more deliberate in their approach to revenue growth, with a focus on executing initiatives that can advance multiple strategic goals efficiently.
For one LHS, an umbrella strategy around growth in retail and commercial pharmacy to drive revenue and growth is broken down intentionally into focused sub-goals. For instance, specialty pharmacy strategies are focused on diversifying revenue and streamlining medication management or prior authorization. Retail pharmacy is focused on improving the patient experience and care outcomes, while mail order pharmacy is specifically grown to gain patient loyalty in new markets.
2. Leaders are in varying stages of the “AI hype cycle."
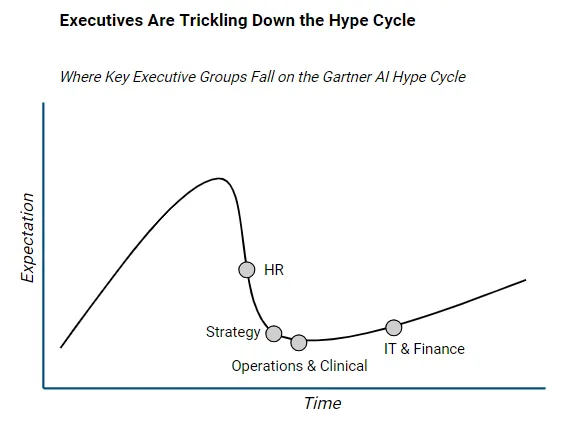
Health system leaders are all in different stages of the “AI hype cycle,” with expectations on AI’s impact varying most between tech and non-tech leaders.
CMIOs discussed how they are managing the expectations of non-tech executive roles, who are seeing AI as a catch-all solution for the workforce and operational problems they are facing.
However, some finance and clinical leaders are starting to feel disillusioned with the “AI hype.”
CFOs are focused on seeing how their pilot results live up to vendor claims, all of which promise sky-high impact.
Many CPE’s are seeing AI-enabled time savings for physicians, but trying to figure out for which clinicians they will see the greatest impact and how to best communicate the changes. Some are wondering how AI will be a differentiator among employers.
Many CNEs feel nurses have been left out of AI productivity savings and want to find solutions.
Generally, health systems are seeing improvements in productivity and reduced cognitive overload in AI pilots. But these results are producing small labor efficiencies that are difficult to plan around.
For example, if a new tool saves a doctor 30 minutes of their time each day, leaders are trying to figure out how that translates to reduced labor costs on a broader scale.
Clinical leaders are also navigating the challenge of getting buy-in from physicians and nurses, which requires having the right messaging and training to ensure full AI adoption.
Early pilot results indicate that physicians perform better when they get more AI training, implying that more training and education still needs to be done to ensure full optimization.
Nurses also remain skeptical of AI, largely because they haven’t been included in the larger decision-making process, and because clinical use cases for AI don’t address the cognitive burden and workflows unique to nursing.
CHROs are playing a role in creating and delivering organization-wide messaging on AI.
3. There is a new sense of urgency to invest in professional development for retention.
CHROs agreed that health systems must be more proactive in recruiting and retaining their workforce than they were pre-Covid.
While turnover in nursing has stabilized to roughly 13%, health systems are still grappling with 30% turnover in entry-level and allied health roles.
High turnover is financially and clinically unsustainable. Therefore, health systems have a new sense of urgency to provide entry-level employees with the professional development programs they need to perform well and envision future career growth within the health system.
HR leaders are specifically focused on providing career coaching and apprenticeship programs.
Both HR and clinical leaders are focused on cultivating a new generation of leaders, with the goal of strengthening succession planning and giving leaders the skills they need to limit turnover.*
Many are providing coaching, peer support, curriculum in a modular, micro-learning format to help leaders quickly learn and apply new skills.
One health system shared survey data that, without a positive wellness-focused leader, over half of providers would leave the organization in two years. Therefore, they focused on how to give clinicians self-assessments on where they may have gaps in supporting staff wellness.
4. Health systems need the board aligned on a proactive cybersecurity strategy.
The rising frequency of cyberattacks is compelling finance and tech leaders to ramp up their cybersecurity infrastructure to protect their finances as well as develop contingency plans.
CFOs and CIOs are focused on building stronger business continuity and cyber response protocols, and training employees on data security measures.
CFO and CSOs are particularly focused on vetting third-party partners to ensure they have the right cybersecurity measures in place. This has limited some enthusiasm for smaller acquisitions of community providers.
However, cybersecurity investments are often costing more than expected—forcing finance and tech leaders to collaborate on board education about the magnitude of cybersecurity risks and building the business case for advancing cybersecurity governance.
Often, cybersecurity efforts require tradeoffs with consumerism goals. Health systems are grappling with the balance between frictionless care experiences for patients, and the sometimes-cumbersome guardrails (e.g., two-factor authentication) needed to ensure their data is protected.
5. Many health systems will drop Medicare Advantage plans in the next year as the strategy of contracting with all plans in the market is growing unviable.
Increased denials, audits and prior authorization have pushed yield on MA contracts to 80-90% on average. This has forced many health systems to reconsider their contracting strategy and evaluate each payer contract with the goal of potentially culling the greatest offenders.
While terminations come with substantial reputational risk, over 60% of CFOs at larger systems and 90% of CFOs at smaller systems (<$2B in TOR) are looking to term MA contracts this year.
There is a consensus among finance, strategy, and clinical leaders that the current headwinds in MA will be highly impactful for health systems that own their own MA plans. Some are looking to limit their plan growth—even if not yet at breakeven scale—given the headwinds.
However, CSOs questioned how much the current headwinds will ultimately impact payers. Some believed they just part of a natural cycle of ebbs and flows, while others believed they will find margin through increasing friction for patients.
Health systems who were relying on their own MA plans to advance other strategies (e.g., value-based care, consumerism, market differentiation, etc.) may need to reevaluate the role MA plays in the future.
For a PDF version of this piece, please click "Download PDF" at the top of the page.
* Note: For those looking for support with leadership development and building the next generation of leaders, please know that The Health Management Academy offers fellowships that prepare high-potential leaders for executive-level positions and a Physician Leadership Program that equips mid-level physician leaders with essential business acumen. Learn more here.
