Auxira Health—a virtual cardiology model initially developed and deployed by MedStar Health as part of its Connected Cardiology program—has officially launched commercially, with plans to rapidly expand nationwide.
The company helps expand cardiology practices by leveraging Advanced Practice Providers who work remotely and handle low-acuity visits and administrative functions like inbox messages. Under the model, each APP (supported by a remote team of MAs and RNs) is matched with up to three cardiologists and undergoes training to fully integrate with the care team.
Auxira’s APPs have prior cardiology experience and are trained side-by-side with physicians onsite before integrating virtually. The remote teams work within the practices’ existing EHR and billing systems—a key selling point for provider partners.
“There's no meaningful IT burden, there's no long-term IT integration. We jump onto their EHRs, and so we feel like a truly white-labeled extension of their care.” – Auxira CEO and Cofounder Inna Plumb
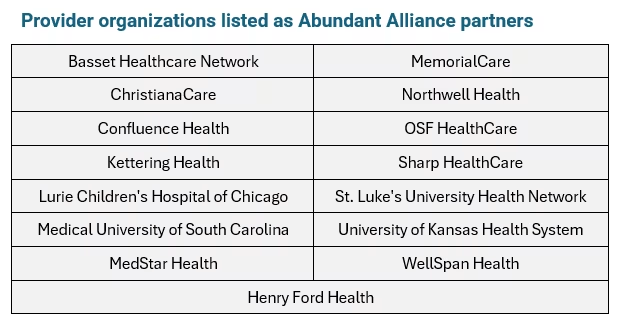
Auxira is backed by Abundant Venture Partners, developers of a collaborative investment platform with more than a dozen health system partners. Auxira also received operational support from Studio Red, the American Heart Association’s venture studio.
MedStar Health has been working on the model for approximately two years and launched the company in stealth last December after bringing PE investor Inna Plumb onboard as CEO. Plumb was a founding partner at Redesign Health, another healthcare startup incubator with health system backing.
The firm faces competition from several other virtual cardiology support and remote care providers, including:
Recora Health, which offers virtual cardiac rehabilitation programs in collaboration with health systems like Davis Health System and UNC Health Rex.
Ventricle Health, a value-based virtual cardiology services provider with undisclosed health system and ACO partnerships.
Story Health, a specialty care platform with patient coaching services that has worked with Intermountain Healthcare and West Virginia University.
Primary care disruptors like Teladoc and Amwell, which have likewise partnered with hospital-based cardiologists to offer remote care capabilities.
Hims & Hers Health launched its own program called “Heart Health by Hims” in 2023 that personalizes treatment plans to simultaneously treat ED and high cholesterol using a single-pill combination therapy.
These competing models typically deliver care through standalone virtual platforms, centralized telehealth clinics, or direct-to-consumer services that operate outside of existing provider workflows—whereas Auxira embeds remote clinical teams directly into cardiology practices.
So What?
Auxira’s launch is an opportunity for health systems looking to expand cardiology capacity, and it’s also a case study for how health systems can leverage their unique expertise in venture investing. Here are some of our top takeaways:
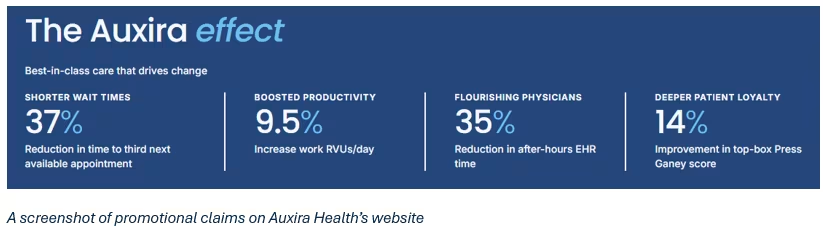
1. Auxira offers a scalable model for cardiology's capacity crunch
Cardiology exemplifies many of the structural challenges health systems face across specialty care: shifting demographics, rising incidence of chronic disease, increasing clinical complexity, and persistent workforce shortages. With an aging cardiologist workforce and limited pipeline growth, systems are working to prevent delays in access, overextended clinical teams, and pressure on both quality and revenue.
In this context, models like Auxira’s represent an emerging strategy for extending capacity without expanding headcount. By integrating remote clinical teams directly into existing workflows, systems can offload high-volume, lower-acuity tasks that often bog down specialty clinics such as patient follow-ups, medication adjustments, and inbox management.
Crucially, this approach doesn’t rely on new technology adoption or parallel platforms. Instead, it seeks to strengthen existing infrastructure by embedding support into the clinical and operational fabric of the practice, offering a pragmatic path to improving throughput, continuity, and staff well-being without overhauling core delivery models.
2. Health systems need to compete on both care quality and convenience
As virtual-first companies and retail health entrants expand their footprint into chronic and specialty care, traditional health systems are under growing pressure to evolve. While these models may not offer the depth of care available in a health system, they are reshaping patient expectations around convenience and responsiveness.
Health systems, in turn, are being challenged to compete not just on clinical quality, but on access, flexibility, and patient experience. The comparative advantage systems hold—longstanding clinician relationships, integrated care environments, and infrastructure for high-acuity needs—can be diluted if front-end access and care navigation fall short.
Embedding scalable virtual support within existing practices is one way to reinforce that advantage. By improving specialty access without removing patients or care from the system, these approaches can help health systems retain clinical control, preserve referral integrity, and modernize service delivery without fragmenting care.
3. Investing collaboratives help health systems leverage their clinical expertise at scale
Auxira’s development through Abundant Venture Partners highlights a broader trend: health systems seeking not just to adopt innovation, but to co-create it. Participating in mission-aligned venture initiatives allows systems to help shape emerging solutions from the outset, ensuring new care models are designed with frontline realities in mind. There’s also strength in numbers: investing as a group can jumpstart adoption at multiple systems and across multiple geographies.
For CSOs, this kind of investment represents more than diversification. It’s a strategic tool for scaling the system’s expertise and influence—a way to bring clinical insight into the innovation pipeline and pilot solutions that reflect the unique needs of their providers and patient populations.
Moreover, involvement in these collaboratives can accelerate internal transformation by exposing leadership teams to new operational models, data frameworks, and care delivery innovations. As healthcare becomes more distributed, digital, and consumer-driven, these partnerships offer a pathway for health systems to extend their strategic reach and shape the future of care on their own terms.
